- About
- Advertise / Support
- Contact
- CancerNetwork.com
- TargetedOnc.com
- OncLive.com
- OncNursingNews.com
- Terms & Conditions
- Privacy
- Do Not Sell My Information
© 2024 MJH Life Sciences™ and CURE - Oncology & Cancer News for Patients & Caregivers. All rights reserved.
Sarclisa Delivered Through Under-the-Skin Injection Shows Promise in Patients With Pretreated Myeloma

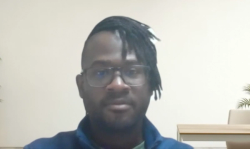
Ryan McDonald, Associate Editorial Director for CURE®, has been with the team since February 2020 and has previously covered medical news across several specialties prior to joining MJH Life Sciences. He is a graduate of Temple University, where he studied journalism and minored in political science and history. He considers himself a craft beer snob and would like to open a brewery in the future. During his spare time, he can be found rooting for all major Philadelphia sports teams. Follow Ryan on Twitter @RMcDonald11 or email him at rmcdonald@curetoday.com.
Delivering Sarclisa via an under-the-skin injection may improve the quality of life of patients with pretreated relapsed, refractory multiple myeloma, according to recent research.
Treatment with Sarclisa (isatuximab-irfc) delivered via an under-the-skin injection through either a syringe or on-body delivery system resulted in similar outcomes compared with intravenous Sarclisa when combined with Pomalyst (pomalidomide) and dexamethasone in patients with relapsed/refractory multiple myeloma, according to recent data.
The findings, according to the study authors, highlight the benefit of a subcutaneous (under-the-skin) injection of Sarclisa versus an intravenous (IV; through a vein or veins) delivery of the drug.
“Subcutaneous delivery of (Sarclisa) would optimize convenience of administration, with the intent to enhance comfort and quality of life of the patients and reduce health care resources,” lead study author Dr. Hang Quach, the director of clinical hematology and clinical hematology research at St. Vincent’s Hospital in Australia, and colleagues wrote in a poster of the data that were presented at the 19th International Myeloma Society Annual Meeting.
Fifty-six patients were enrolled into the multicenter, phase 1b trial in an effort to analyze the safety, pharmacokinetics (how the drug moves throughout the body) and efficacy of an under-the-skin injectable version of Sarclisa compared with Sarclisa plus Pomalyst and dexamethasone delivered through an IV into the patients’ veins.
Assessing the safety of the treatment method, including the amount of dose-limiting side effects and injection-site reactions were the main goals of the study. Of note, an injection-site reaction may include pain, itching, swelling or redness around the area where the medication was injected. According to information posted on the UC San Diego Health website, most injection-site reactions aren’t serious and go away on their own.
The investigators also reviewed the effects on overall response rate (percentage of patients whose disease responded to treatment) and progression-free survival (time from first treatment until disease worsens).
Patients received the study drug either through their veins (12 patients), under the skin injection via syringe (22 patients) or through an on-body delivery system (22 patients).
The on-body delivery system was a wearable device placed on the abdomen by a medical professional.
As of Jan. 20, 2022, eight of the 12 patients receiving Sarclisa plus Pomalyst and dexamethasonethrough their vein discontinued treatment. Seven of the discontinuations were attributed to disease progression while the other patient voluntarily withdrew from treatment. In total, 17 of the 44 patients who received Sarclisa via an under-the-skin injection had discontinued their therapy.
The findings showed that patients within the group that received Sarclisa plus Pomalyst and dexamethasone achieved an overall response rate of 66.7%. Among 32 evaluable patients in the Sarclisa injected the skin group, the combined overall response rate was 78.1%.
The estimated median progression-free survival for the patients in the group that received treatment into their veins was 22 months. However, the estimated median progression-free survival among the 32 patients evaluated or overall response had not yet been reached. Of note, a median progression-free survival that has not been reached means that more than half of the patients in the group remain alive without disease progression at the time of the last data review.
The rate of the treatment-related side effects that were serious or severe were comparable across the patient groups, according to the findings.
Every instance of infusion or injection reaction was considered to be moderate and only occurred following the first treatment.
All the patients in the intravenously delivered group had a serious or severe treatment-related side effect. More than 90% of the patients in each group that received Sarclisa delivered via injection under the skin developed a serious or severe treatment-related side effect.
“(Sarclisa) subcutaneous administration by on-body delivery system is well tolerated, requires a short duration of injection, and provides a convenient, hands-free option,” the study authors concluded.
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.
Related Content: