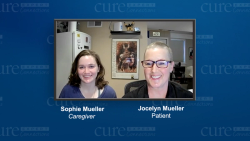
HER2-positive Breast Cancer: Jocelyn’s Story - Episode 1
An Overview of HER2-positive Breast Cancer
Julie Fisher, MD, gives a brief overview of HER2-positive breast cancer and the tests available for diagnosis.
Julie Fisher, MD: Hello, and welcome to Cure Expert Connections on HER2-positive breast cancer. I'm Dr Julie Fisher and I'm a medical breast oncologist at the Levine Cancer Institute in Charlotte, North Carolina. I'd like to welcome one of my patients, Jocelyn Muller, who's here today to share the story of her journey with HER2-positive breast cancer. Welcome, Jocelyn. We're going to spend the next 60 minutes walking you through her diagnosis, treatment, and follow-up from each of our perspectives and our continued communication throughout the process.
Let me just go ahead and open with a brief overview of HER2-positive amplified breast cancer. This is referring to the human epidermal growth factor 2 receptor. This is a protein that is expressed on the surface of all breast cancer cells. It is overexpressed or present in excess in roughly 15% of cases of breast cancer. This is diagnosed via biopsy, so if a patient presents with an abnormal finding on her routine mammogram or if she's able to palpate an area of abnormality and is then referred for a biopsy, that's the next thing that happens. That is typically done these days in our radiology departments. They numb the skin, place a hollow bore needle in the tumor itself, and obtain some tissue. Our colleagues in pathology then look at the tissue under the microscope and can ascertain if it is indeed breast cancer. Anytime someone is diagnosed with an invasive breast cancer, the pathologists first test for the presence of the estrogen and progesterone receptors. They also assess this HER2/neu protein to determine: is this one of the cases that is overexpressed and has excess protein? Or is this indeed a case where there is the standard amount of HER2/neu protein? Again, the roughly 15% of cases that overexpress HER2/neu are referred to as HER2/neu-amplified or HER2/neu-positive; this is very relevant for the physician team taking care of the patient with HER2-amplified breast cancer because it has significant implications for both prognosis and treatment. We know that HER2-positive breast cancer has the potential to behave more aggressively, and it has a higher risk of returning post-treatment. Historically, that was something that we could only lament, but thankfully that changed dramatically in the early part of the 2000’s with the advent of drugs that specifically target that HER2/neu protein. I tell my patients, "We use those drugs in conjunction with chemotherapy." I think of those specially target drugs, such as snipers, and they're going to specifically home-in on that overexpressed HER2/neu protein. That has again dramatically changed the landscape of how we treat HER2-amplified breast cancer. It's changed this from a disease that we previously thought was very high risk, into something that we have wonderful tools for treating. Again, these account for about 15% of breast cancers. Most HER2-amplified breast cancers will be hormone receptor-positive, meaning sensitive to either estrogen, progesterone, or both. The minority of those cases will be insensitive to those hormones but overexpress the HER2/neu protein. That has an effect on subsequent treatment recommendations as well. How do we test for this? There are 2 main ways that our pathology colleagues assess HER2/neu positivity. One is a simple stain: it's a test referred to as immunohistochemistry. Another scientific method for determining HER2/neu status is what we call FISH, which stands for fluorescence in situ hybridization. Either of those 2 tests can garner a HER2-positive breast cancer diagnosis.
Transcript edited for clarity.