- About
- Advertise / Support
- Contact
- CancerNetwork.com
- TargetedOnc.com
- OncLive.com
- OncNursingNews.com
- Terms & Conditions
- Privacy
- Do Not Sell My Information
© 2024 MJH Life Sciences™ and CURE - Oncology & Cancer News for Patients & Caregivers. All rights reserved.
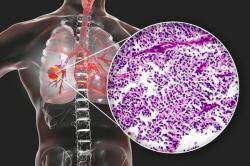
A View From a Young Lung Cancer Survivor: Genomic Testing Provides Hope
To gain a patient's perspective on the Genomics of Young Lung Cancer Study and the importance of genomic testing, we spoke with Corey Wood, a 23-year-old trial participant and lung cancer survivor.
Researchers have long been confounded by the incidence and causes of lung cancer in young individuals who never smoked. An estimated 4,500 people under the age of 45 were diagnosed with the disease last year.
In July 2014, the Addario Lung Cancer Medical Institute, a partner of the Bonnie J. Addario Lung Cancer Foundation, facilitated the launching of a first-of-its-kind study to answer this question.
To gain a patient’s perspective on the trial and the importance of genomic testing, CURE spoke with Corey Wood, a 23-year-old trial participant and lung cancer survivor from Yorba Linda, California.
CURE: Could you tell me a little bit about your life before your diagnosis and then about the diagnosis?
Wood: I was in school at the University of California, Berkeley, right before the diagnosis. I had always been an athlete and I come from an outdoorsy family. At the time, I was really into marathons and triathlons. It was my senior year and I had a job set up in Denver.
I had this slight flash in my right eye that I only mentioned to the doctor because I was having my contact prescription renewed. He said to come back in a month to see if the flash grew. When I thought the flash got a little bigger, I was transferred to a retina specialist and then to an eye tumor specialist. It was that eye tumor doctor who ordered a full-body scan. I had internships, I had races, I had school, I had work — I was very distracted and thought I was just going through the motions by doing the full-body scan. I never once thought it was cancer.
After I got the diagnosis, it probably took a week for me to actually accept and think, “Oh, I have stage 4 lung cancer.” It was just so, so unexpected.
I started to do some research and the Internet was devastating at first. Then, I started reading about targeted therapies and genomic tests that could be done. My initial needle biopsy had actually already been submitted for EGFR and ALK mutations.
After two weeks, they both came back negative and I thought I was just done there. I wasn’t sure if chemotherapy was going to work.
Luckily, my doctor, Timothy E. Byun, had a feeling that I had to have a mutation [editor's note: Byun is an oncologist at St. Joseph Hospital in Orange, California].
“You’re so young, you have to have a mutation,” he said. “Can I schedule you for surgery and remove one of your larger nodules to submit?”
It moved quickly then. I found out I was positive for ROS1, picked up my Xalkori (crizotinib) pills three days later and about three months later, the cancer was completely gone: clear lungs, clear lymph nodes and the bone metastases were healing. I was able to get back to running to keep me mentally sane — a normalcy I know a lot of other survivors don’t get to experience.
This past May, I had a typical PET/CT scan and brain MRI. My body came back clear but I had my first go-around with brain lesion so I switched targeted therapies to the investigational drug entrectinib (RXDX-101) in June.
My biggest lesion is 5 mm, so we don’t have to go a lot to go off of but it hasn’t grown at all, and I don’t have any new spots. My body is still clear. I’m going to stick with this drug for a bit and keep my eye on some other ones that are doing well in trials.
I’ve been feeling really good lately — I’ve stopped taking my stimulants and my laxatives. No rash anymore, no itchiness. No fatigue — that’s the best part.
I’m also moving to Denver in three weeks, I just had my second interview for a job and I’m about to buy a car. Life is moving forward finally.
How did you hear about the Genomics of Young Lung Cancer Study?
I heard about it from Emily Bennett Taylor — we had the same oncologist. After I started Xalkori and kind of got the hang of treatment, I ended up switching oncologists to be at a research facility.
I switched to Karen Reckamp, who does work with the Bonnie J. Addario Lung Cancer Foundation [editor’s note: Reckamp is the co-director of the Lung Cancer and Thoracic Oncology Program at City of Hope].
Dr. Reckamp said I should reach out to Emily because she might be able to offer some emotional support. Emily and I ended up meeting for lunch soon after and, most of the time, we talked about things other than lung cancer. She did tell me about the Young Lung study and right away I said, let’s do it — What do I need to sign? How can I get involved?
Do you think genomic testing is crucial for all patients with lung cancer?
Yes. If I would have stopped after that first ALK/EGFR test, who knows where I would be now.
It was mostly a psychological thing, for me. With a drug that was made for my ROS1 mutation, I thought, “OK, I think I’m going to live now.”
I’m glad I got a full test and didn’t just stop after the common ones.
What do you think the impact of the Young Lung study has been?
There’s definitely more awareness of genomic testing now. Testing gives us hope, especially to us young people. It’s nice to know that young people aren’t being treated the same as everyone else. What does it mean to you, personally, to be involved with the study? It feels good. It’s nice to leave a footprint. I know that it’s a small population of patients with lung cancer, but I see the bar graphs as individuals. I can put faces to the numbers in the study and I hope that makes a difference to the researchers.
Do you think there’s enough attention being paid to young patients with lung cancer?
No, we still have this huge problem that people think you have to have smoked to get lung cancer. My friends are still baffled by it. At this point, I’m not as baffled because I’ve met so many of us. It gets frustrating sometimes. I’d like more attention to be paid to young lung cancer patients, to us ROS1ers, and to non-smokers. I think we have a ways to go.
How else are you trying to leave your footprint and help patients with lung cancer?
My blog is coming full circle. Before my diagnosis, I was a pretty private person. I started my blog, though, because it was exhausting to give people the same update over and over again. I just couldn’t do it anymore. I made a blog and I would just tell people to read it to know how I’m doing — it was the best decision ever. Now I’m at the point where other people in their 20s are reaching out to say that they’re in the same situation and asking if we can talk. That feels good — to be to someone else what Emily was to me.
What advice do you give to those people?
I tell them to never lose hope and to focus on what’s happening. I’ll joke with them that — because of mutation testing and new treatments — now’s the time to get lung cancer ... if you had to.
Related Content: